Unfolded Protein Response pathway offers new targets to treat bone weakness in cancer patients
New drugs that modulate protein processing in bone cells may prevent bone weakening and limit the growth of bone-localized tumors
CHINA, September 25, 2025 /EINPresswire.com/ -- The unfolded protein response (UPR) is a protective pathway that helps cells manage stress during protein production. Cancer cells exploit this system to survive harsh tumor environments. In bones, they also disrupt the balance of bone-building and bone-resorbing cells, leading to skeletal fragility. Emerging therapies that target the UPR show promise in restoring bone health while selectively killing malignant cells, offering new hope for patients with cancer-associated bone disease.Before a chain of amino acids can become an active and useful protein, it must be processed and folded into the appropriate conformation. Much of this processing occurs in the endoplasmic reticulum (ER) of every cell. However, any disruptions in protein homeostasis can be very stressful to the ER, and when the ER gets overwhelmed, a safety system called the Unfolded Protein Response (UPR) engages to slow down protein synthesis and allow the ER to catch up. If a temporary slowdown of protein synthesis isn’t enough to restore normal ER function, the UPR triggers cell death.
In many types of cancerous cells, the UPR response is altered to prevent cell death and drive the relentless growth that characterizes malignancy. These changes allow cancerous cells to tolerate the low oxygen and low nutrient environment of a tumor and continue to multiply. Drugs and therapies that target parts of the UPR pathway could therefore be effective against several types of cancers.
Professor Sarah A. Holstein and Dr. Molly E. Muehlebach from the University of Nebraska Medical Center have thoroughly examined how the UPR pathway relates to cancer-induced damage in bones. In their review paper published online on 28 August 2025 in Bone Research, Prof. Holstein and Dr. Muehlebach examined existing research on how the UPR pathway is deeply connected with the differentiation of cells in bone tissue, the maintenance and renewal of bones, and how infiltration of bone by cancerous cells hijacks the UPR pathway to cause structural weakening of bone. This occurs for cancers such as osteosarcoma and Ewing sarcoma (primary bone cancers), as well as blood cancers like multiple myeloma and solid tumors that metastasize to bone, such as breast or prostate cancer.
Discussing the importance of this research, Prof. Holstein says, “Disruption of the remodeling cycle can result in bone loss or increased bone density. However, in both cases, the bone is brittle and can easily fracture. As a result, skeletal structure and integrity is compromised, significantly contributing to disease morbidity and negatively impacting overall patient survival in cancer-induced bone disease.”
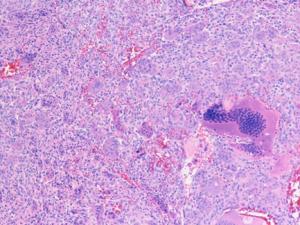
In their paper, Prof. Holstein and Ms. Muehlebach first look at the three primary UPR pathways – Eukaryotic translation Initiation Factor 2 Alpha Kinase 3 (EIF2AK3); ER to Nucleus signaling 1 (ERN1); Activating Transcription Factor 6 (ATF6) and their downstream cascades. They then describe the specific roles of many UPR-associated proteins in the differentiation of osteoblasts (bone-building) and osteoclasts (bone-dissolving) cells from skeletal stem cells. Healthy bones require both kinds of cells to work in an optimal fashion. However, when cancerous cells invade bone tissue, they induce UPR-associated dysfunction of osteoclasts, osteoblasts, or both, resulting in bones that are either weak due to lack of density or brittle due to excessive mineralization. These phenomena are termed “skeletal related events” (SREs).
Emerging classes of drugs may reduce SREs by targeting specific aspects of each of the three UPR cascades and their downstream proteins. The mechanisms of action against SREs include:
• Inhibiting EIF2AK3 (e.g. GSK2606414)
• Inhibiting ERN1 (e.g. Sunitinib malate, Toyocamycin)
• Inhibiting disruption of ER associated protein degradation (e.g. VCP inhibitors such as CB-5083)
• Enhancing chaperone proteins to increase folding rates and relieve ER stress (e.g. Sodium phenylbutyrate)
Other emerging drugs with high affinity for bone tissue induce UPR-mediated apoptosis in malignant cells by:
• Disrupting the synthesis of isoprenoids needed for protein processing (e.g. bispho- sphonates zoledronic acid (ZA), RAM2061)
• Disrupting the degradation of unfolded proteins (e.g. Oprozomib)
All of these drugs are at various stages of in vitro, animal, or early human trials, and show various degrees of promise in alleviating SREs and killing tumors localized in bones. Much work remains to be done, however, to ensure that these UPR modulating drugs act in a targeted manner against cancerous cells, and do not disrupt other functions within bone or other tissues.
As Prof. Holstein concludes, “Ultimately, the success of UPR modulators in treating cancer-related bone disease will depend on developing agents that specifically target bone and tumor cells while minimizing effects on healthy tissue.”
***
Reference
Title of original paper: The role of the Unfolded Protein Response pathway in Bone Homeostasis and potential therapeutic target in Cancer-associated Bone Disease
Journal: Bone Research
Authors: Molly E. Muehlebach and Sarah A. Holstein
DOI: 10.1038/s41413-025-00457-6
About the University of Nebraska Medical Center
Established in 1869, the University of Nebraska Medical Center (UNMC) is a public research university and health center located in Omaha, NE, USA. The university currently houses a hospital as well as colleges for dentistry, pharmacology, nursing, medicine, public health and allied health professions. In recent years, UNMC was involved at the forefront of the United States’ response to the 2014 Ebola epidemic and the 2020 SARS-CoV-2 pandemic. As of 2025, UNMC serves over 4,000 students and has strong research links with other institutions in the University of Nebraska system.
Website: https://www.unmc.edu/
About Professor Sarah A. Holstein from the University of Nebraska Medical Center
Prof. Sarah A. Holstein is a Professor in the Division of Oncology and Hematology at the University of Nebraska Medical Center (UNMC). She completed her MD and PhD, as well as clinical training in hematology/oncology from the University of Iowa (UI), before serving as a faculty member at the UI and then Roswell Park Comprehensive Cancer Center. She joined the faculty at UNMC in 2016. Her basic science, translational and clinical research focuses on multiple myeloma. Prof. Holstein has published over 140 research articles and book chapters. In addition to her research, she serves on the International Myeloma Working Group as well as several national myeloma committees and is an Associate Editor for Clinical Pharmacology and Therapeutics.
Yini Bao
Bone Research Editorial Office
+862885546461 ext.
email us here
Visit us on social media:
X
Legal Disclaimer:
EIN Presswire provides this news content "as is" without warranty of any kind. We do not accept any responsibility or liability for the accuracy, content, images, videos, licenses, completeness, legality, or reliability of the information contained in this article. If you have any complaints or copyright issues related to this article, kindly contact the author above.